The following information and more can be found at https://www.ossur.co.za/prosthetic-solutions/information-for-amputees
Life after amputation
An amputation is a traumatic and life changing experience for any individual. Being informed about the rehabilitation process after amputation may lead to better acceptance for the patient.
Why are leg amputations done?
The most common cause for amputation is due to vascular disease which includes diabetes. According to data from the USA, vascular disease contributes to 54% of lower limb amputations. Other reasons include, trauma, cancer and congenital deformities.
So what about life after amputation?
Preparing for a life with amputation
If you’ve prepared yourself well, you’ll understand why the amputation is necessary, and will realise that even though an artificial limb can’t ever be the same as a natural limb, it will probably be a whole lot better than a non-functional or diseased limb. Knowledge puts you at an emotional and even medical advantage: it reassures you, aids your recovery and ultimately helps you fight your fears. This is why we say that the better you understand why you need an amputation, what happens during surgery, and what the recovery and rehabilitation are expected to entail, the better you’ll be able to deal with the consequences of losing a part of your body.
After amputation surgery
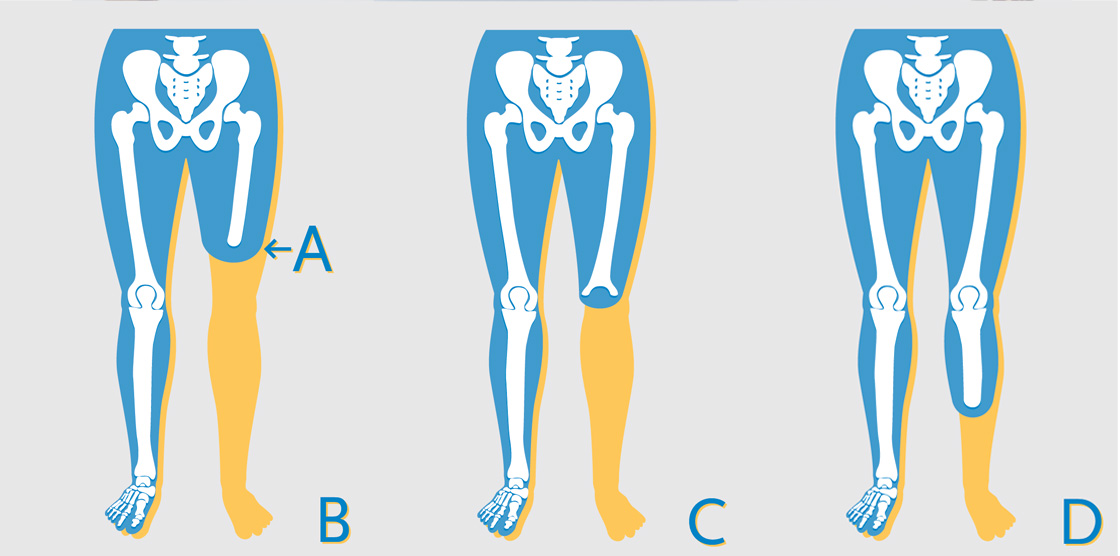
A “typical” lower-limb amputation can broadly be divided into three phases, namely the wound healing phase, the mobilisation phase and the reintegration phase. But please remember: every person is unique, and treatment methods differ. This means that the steps we describe may not coincide exactly with your own treatment pathway.
Wound healing
The wound healing phase after amputation consists of the time it takes for the wound or incision site to close and heal.
It’s very important to remember that the healing time after surgery varies from person to person and the length of your recovery period depends on all kinds of factors, such as the reason for your amputation, your age, health and the rehabilitation protocol followed by your medical team.
Shaping of the residual limb
When the surgeon is satisfied with how the wound is healing, compression therapy can begin. The aim here is to shape your residual limb, because this has a direct bearing on the successful fitting of a prosthetic leg: a residual limb with an even, uniform shape will present fewer complications when you’re eventually fitted with a prosthetic leg. The method most commonly used is with compression bandages. These are special bandages that are applied to the residual limb in a specific way to shape the limb.
After the coning phase a silicone liner is used for shaping before the prosthetic fitting stars.

The mobilisation phase
As soon as your surgeon feels you’re ready, a physiotherapist will help you mobilise your body with special exercises. Early mobilization is very important: it has been proved that in general the earlier one is mobilized, the faster recovery happens. At this stage, your residual limb is probably still being shaped with post-operative silicone liners, and you’ll be carefully monitored to see when you’re ready for the reintegration phase. When the wound has healed sufficiently, the surgeon will discharge you from hospital, and you’ll continue the mobilisation exercises until you’re ready for the first fitting of a prosthetic leg.
The reintegration phase
The goal of the reintegration phase is to restore your mobility and independence as fully as possible. Working with a team of well-coordinated experts will increase the quality of your care and significantly reduce the duration of your rehabilitation. Consulting with a prosthetist is a good way to start on the road to recovery, but you will most likely also need help from other medical professionals, such as a physiotherapist, a biokineticist, a psychologist, an occupational therapist and perhaps even a dietitian.
This type of multidisciplinary team is available in specialised rehabilitation centres in some areas, but if you live in a small town or a rural area, there may not be enough patients to support such a facility. If you can, it might be a good idea to invest in your health by commuting to a rehabilitation centre until your independence is restored.
When you undergo amputation surgery, you are profoundly challenged at every level of your being – physical, emotional, mental and spiritual. The indisputable fact is that your limb is permanently gone. How you respond to that reality depends on whether or not you give in to despair, and will determine whether you grow as a human being and heighten your appreciation of living.
The real challenges that accompany the loss of your limb cannot be made to disappear, but, through rehabilitation, their negative effects can be minimized. The word “rehabilitate” means “restore”. After surgery, your rehabilitation goal should be to restore your body, mind and spirit.
Once the wound has healed and you’re ready to be fitted with your new prosthesis, the prosthetist becomes a central figure in your further recovery and reintegration. In fact, a prosthetist will play an important role in helping keep you mobile for the rest of your life. So you can see why choosing a prosthetist is one of the most important decisions you need to make.
How do you know which prosthetist to appoint? It’s important to remember that you have a choice: South Africa is blessed with some world-class prosthetists. By the time you get to this point, you may already have had contact with a prosthetist referred to you by a doctor and started the rehabilitation process with compression therapy to shape your residual limb. This is good, as it means that you’ve been getting specialist care right from the beginning, which will enhance your recovery, but remember: you aren’t obliged to work with any particular medical practitioner. You may want to continue with the prosthetist who has been treating you up to now, but you might also like to consider another prosthetist. Or perhaps you haven’t had any contact with a prosthetist yet.
Evaluation
Generally, the sooner your prosthesis is fitted, the shorter your rehabilitation is likely to be, so once you’ve appointed a prosthetist, the design and manufacture of your first prosthesis should begin as soon as possible.
The first step is a thorough evaluation in which the prosthetist reviews your physical condition, specifically the condition of your residual limb and whether it has healed sufficiently to accommodate the pressures of the prosthesis on your skin. The evaluation will include your lifestyle requirements, with questions like these:
- Do you have an office job, or is your work more physically demanding?
• Do you walk mainly indoors?
• Are the areas around your house and work flat, or are there many slopes?
• Do you often climb stairs?
And so on. These questions are important, because the answers will help the prosthetist decide what types of components to include in the design of your prosthesis. For example, some components are designed to support less active people struggling to maintain the ideal balance of safety, comfort and mobility, and others for people who are keen to become increasingly mobile. The prosthetist takes all of this and more into account in trying to design the best prosthetic leg for you.
Capturing the shape of the residual limb
The next step for the prosthetist is to capture the shape of your residual limb and take measurements for the prosthesis. This may happen during the initial evaluation, or during a next appointment, depending on when you appoint the prosthetist, the prosthetist’s schedule and so on. Capturing the shape can almost be described as developing a “blueprint” for your residual limb so that a well-fitting, comfortable socket can be designed, taking the unique shape of your residual limb into account. As this is the basis of the suspension for the prosthesis – in other words, where the prosthetic leg is attached to your residual limb – it’s vitally important to capture the shape accurately. Soft tissue changes shape when pressure is applied, which makes this is one of the hardest parts of the prosthetist’s job − and explains why choosing an experienced prosthetist can make a big difference to your life. It helps if the residual limb is shaped in a way that makes designing a socket simpler, which is why we emphasise the correct post-operative treatment during the wound healing phase.
There are various ways of capturing the shape of the residual limb such as casting directly on the residual limb with an air pressure system, or by using digital scanners, but the most common method is to apply plaster of Paris to get a cast of the limb.
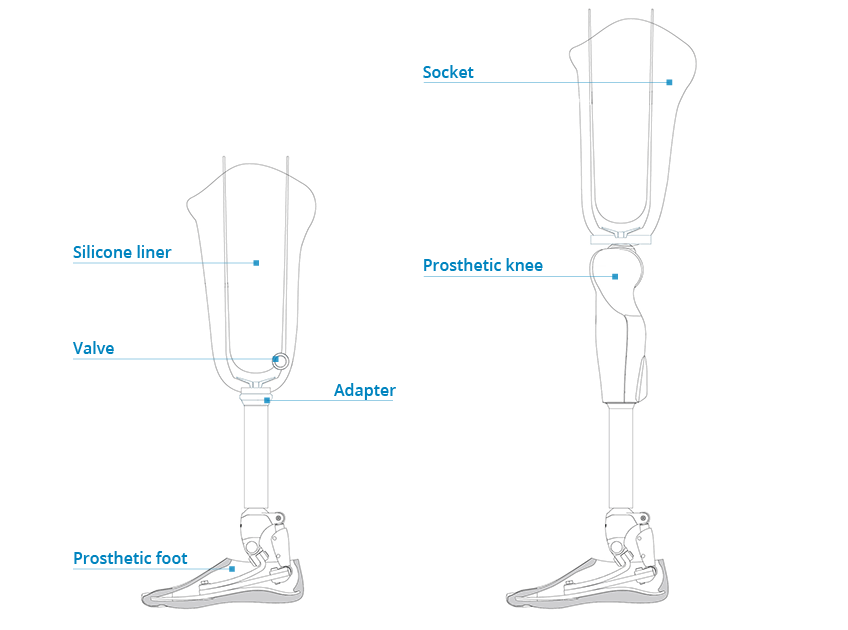
Fitting the diagnostic socket
Using the shape taken from the cast, your prosthetist will now manufacture a diagnostic or “test” socket to evaluate whether that shape will fit comfortably to your residual limb. The diagnostic socket is typically fitted at the following appointment, as it takes time for the socket to be manufactured, modified and perfected before the final socket is made. The test socket is made from a transparent plastic material, not intended for permanent use, but able to adjusted. Once you and the prosthetist are both satisfied with the design and the comfort of the fit, prosthetic components will be assembled and aligned with you in a standing position, a process called “static alignment”. If the result is a stable, comfortable prosthesis, you should soon be able to take your first steps!
Learning to walk
Think of your first steps as a learning experience: some people walk well right from the beginning, but most take time. It’s all part of the journey to reach your own potential. There’s no need to rush: use this phase of the rehabilitation process to get to know how your prosthetic leg works and how your body interacts with it, and ask all the questions you need. Accept that you’ll have to work hard to regain your independence, because disciplined exercise is a vital part of regaining mobility. It’s also normal to experience some pain and discomfort during the first month after surgery, but know that as your limb heals, walking will become more and more comfortable.
Early gait training under the close supervision of a physiotherapist, biokineticist and/or prosthetist is essential so that you learn to walk in the best possible way. Learning to walk with a prosthesis requires you to adopt new techniques; and it’s far better to develop a good walking technique from the outset than to try to correct an inefficient technique later. Your physiotherapist or biokineticist, assisted by your prosthetist, will recommend special exercises aimed at training the specific muscles needed to walk with your prosthetic leg. Typical exercises are illustrated here, but please remember that they are just suggestions and may not be the best exercises for your specific circumstances. Always follow the advice given by the medical professionals in your team, because they have made an expert physical assessment of your individual situation.
Fitting the final prosthesis
The residual limb will go through a process of healing and changing shape as it stabilises over time. This is due to a combination of factors, the main one being fluid changes in your body. The muscles in the limb will atrophy (shrink) since they aren’t functioning the way they used to, you may gain or lose weight, and you may lose muscle tone. However, once you start walking again, you’ll build back some of that muscle tone and might return to your normal weight. Because your residual limb will continue to change shape, the socket attaching your prosthetic leg to it will, at some point, no longer fit perfectly. As you can imagine, a socket that doesn’t fit well may move around, which could have a negative effect on aspects like your safety, energy consumption and comfort. There are ways to manage this temporarily, for instance by putting extra socks over your residual limb, but eventually a new, correctly fitting socket has to be made. Depending on how much your residual limb changes shape, this might have to be done several times, but eventually the limb will stabilise − and at this point a long-term socket can be manufactured for your prosthesis.
Follow-up
Although this long-term socket should fit properly for much longer than the initial, temporary socket(s), you’ll have to get updated sockets made at regular intervals in future. Some adjustments may also be needed now and then as your ability and activity increase and your body adjusts. This process has no clear, predefined conclusion, and there is never a “final leg”, simply because your body is a dynamic system that changes over time, and also because prosthetic components have a limited life. How long the interval between each new socket will be is difficult to predict and varies from patient to patient, but typically it could be three years, with minor adjustments possibly having to be made in between. Please remember, a correctly fitting, comfortable socket is critically important, and you should always give this top priority.
The fitting and manufacture of the prosthesis is both a science and an art, but the two most important aspects of a good prosthesis are indisputably the design of a well-fitting socket with optimal suspension and the correct alignment of the prosthetic components in relation to the residual limb. A good prosthetist always takes special care to make a socket that fits your residual limb perfectly and ensures that the components are aligned correctly.


